USA Revenue Cycle Management (RCM) Market Outlook to 2028
Region:North America
Author(s):Yogita Sahu
Product Code:KROD2156
October 2024
80
About the Report
USA Revenue Cycle Management Market Overview
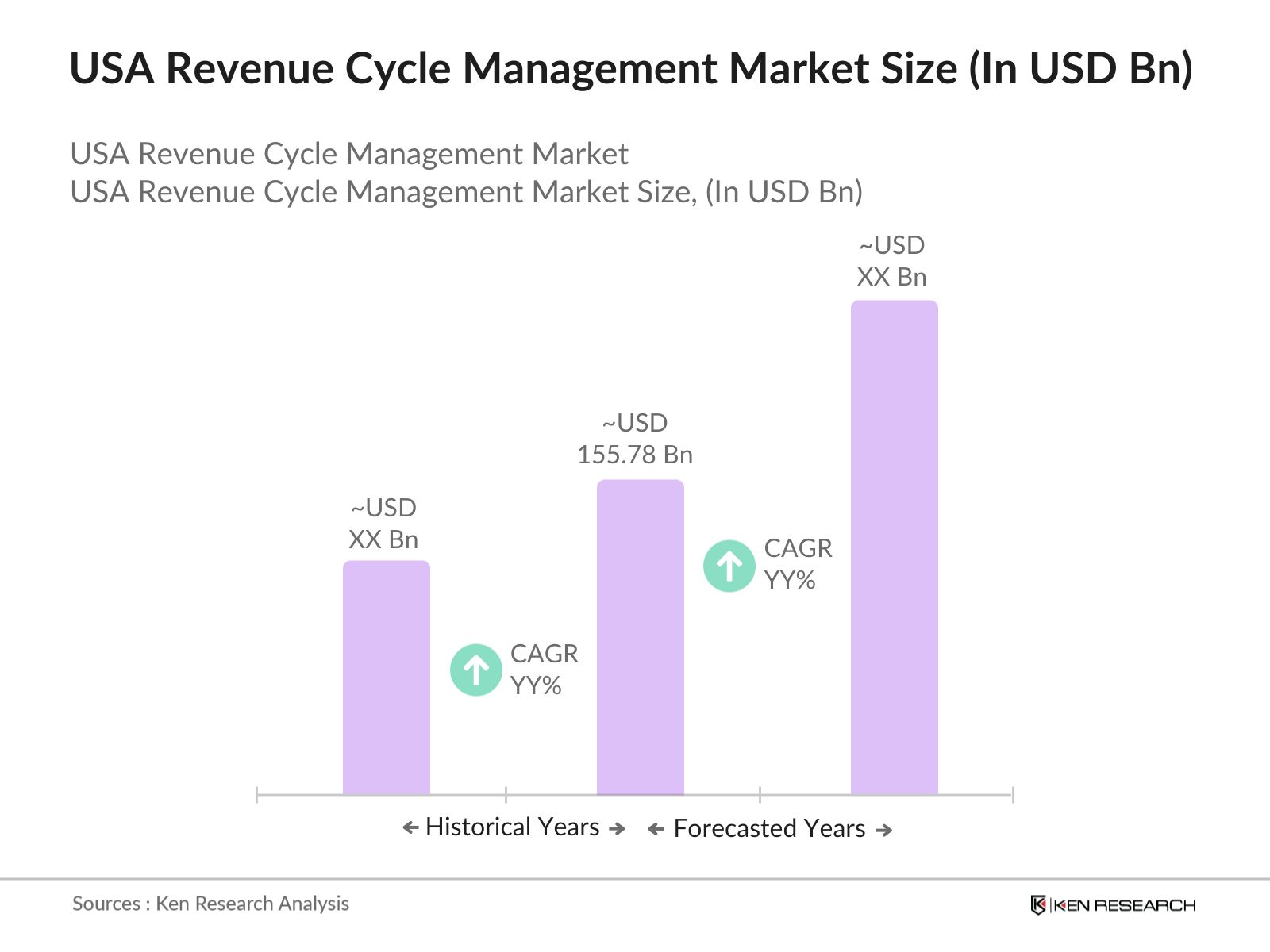
- The USA Revenue Cycle Management (RCM) Market was valued at USD 155.78 billion. The market growth is driven by the increasing complexity of healthcare reimbursements, government regulations, and the rising need for effective financial management in healthcare institutions.
- Major players in the market include Cerner Corporation, McKesson Corporation, Optum360, Allscripts Healthcare Solutions, and GE Healthcare. These companies offer comprehensive solutions that cover end-to-end revenue cycle management processes, from patient registration to final payment collection.
- In September 2023, Cerner and AKASA partnered to offer Cerner customers AI-driven revenue cycle automation. This collaboration allows Cerner users to streamline operations with AKASAs machine learning tools, automating over 25,000 monthly activities for health systems like Methodist Health, which saw a $30 million increase in gross yield.
- In 2023, California emerged as the dominant region in the market, the state's large healthcare infrastructure, coupled with early adoption of advanced healthcare technologies, has driven this dominance. Additionally, major healthcare providers in California have actively invested in RCM solutions to cope with the regions high patient volume.
USA Revenue Cycle Management Market Segmentation
The market is segmented into various factors like product, end-user, and region.
By Product: The market is segmented by product into Integrated Solutions and Standalone Solutions. Integrated Solutions lead the market by the demand for comprehensive platforms that unify various revenue cycle processes, from patient scheduling to final payment collection.

By End-User: The market is segmented by end-user into Hospitals, Ambulatory Care Centers, and Physician Practices. Hospitals held the largest market share due to their larger patient base and more complex billing structures, which require robust RCM systems.

By Region: The market is segmented by region into North, South, East, and West. The West region, held the highest market share due to its advanced healthcare infrastructure, larger healthcare providers, and early adoption of new technologies.
USA Revenue Cycle Management Market Competitive Landscape
|
Company Name |
Establishment Year |
Headquarters |
|
Cerner Corporation |
1979 |
North Kansas City, Missouri |
|
McKesson Corporation |
1833 |
Irving, Texas |
|
Optum360 |
2013 |
Eden Prairie, Minnesota |
|
Allscripts Healthcare Solutions |
1986 |
Chicago, Illinois |
|
GE Healthcare |
1994 |
Chicago, Illinois |
- Optum360: Optum expanded its presence in the RCM market by integrating advanced analytics and care management into its offerings. Notably, in its deal with SSM Health, Optum's analytics aim to reduce care variation and length of stay (LOS), showcasing its strategy to enhance hospital financial performance.
- Athenahealth: Adonis, an AI-powered revenue cycle management (RCM) solution, has joined athenahealth's Marketplace program to enhance healthcare financial outcomes and patient experiences.The partnership aims to leverage AI technology to streamline RCM processes, reduce administrative costs, and improve patient satisfaction.
USA Revenue Cycle Management Market Analysis
Market Growth Drivers
- Increasing Complexity of Healthcare Billing and Reimbursement: The U.S. healthcare system has witnessed a sharp rise in administrative complexity due to changing payer regulations and reimbursement models. The growing demand for seamless, automated billing systems to reduce administrative strain has led to increased adoption of AI-based RCM solutions. This trend is expected to continue as more hospitals and healthcare organizations prioritize operational efficiency to maintain profitability, leading to higher investments in RCM technologies.
- Transition to Value-Based Care Models: In 2024, value-based care continues to grow, with 13 million Medicare beneficiaries under ACOs or value-based arrangements in 2023. The CMS Innovation Center targets 100% of Medicare beneficiaries to be in accountable care relationships by 2030, driving higher demand for effective revenue cycle management solutions. The transition to value-based care has created a growth opportunity for RCM vendors offering solutions that integrate patient data, billing, and quality outcomes.
- Adoption of AI and Automation in RCM: The U.S. healthcare system is increasingly adopting AI and automation technologies to streamline billing processes and reduce manual errors. By 2024, nearly 80% of healthcare providers in the U.S. are expected to incorporate AI-driven RCM solutions, leading to better revenue management outcomes. Automation of tasks such as claim submission, denial management, and patient billing helps healthcare organizations reduce operational costs and improve financial performance.
Market Challenges
- High Costs of Implementation: One of the primary challenges faced by healthcare providers is the high cost of implementing RCM systems. The average cost of deploying a full-scale RCM platform for a large hospital range from $500,000 to $800,000. Smaller healthcare institutions, such as clinics, often struggle to afford these systems due to limited budgets.
- Data Security and Privacy Concerns: With the increasing adoption of cloud-based RCM solutions, data security and privacy have emerged as major concerns for healthcare providers. In 2024, the U.S. healthcare sector is expected to see over 40 million data breaches, exposing sensitive patient information and financial records. This puts healthcare organizations at risk of financial losses and legal liabilities.
Government Initiatives
- Healthcare Transparency Initiative 2023: In 2023, the U.S. government launched the Healthcare Transparency Initiative, mandating hospitals to publicly disclose pricing information for healthcare services. This initiative aims to reduce billing errors and improve patient access to accurate cost estimates. By 2024, compliance with these regulations is expected to increase transparency and reduce disputes over medical bills.
- Medicare and Medicaid Payment Reforms: The U.S. government has introduced several reforms in 2023 to streamline Medicare and Medicaid payments. These reforms focus on reducing the administrative burden on healthcare providers and improving the efficiency of reimbursement processes. RCM systems that can automate and expedite Medicare and Medicaid claims will see increased demand, particularly among healthcare organizations that rely heavily on government reimbursements.
USA Revenue Cycle Management Market Future Outlook
The future trends in the market include the widespread adoption of AI-powered systems, increasing outsourcing of RCM services, integration of blockchain for secure billing, and a shift toward cloud-based RCM platforms.
Future Market Trends
- Widespread Adoption of AI-Driven RCM Solutions: Over the next five years, the adoption of AI-driven RCM solutions is expected to accelerate, with 90% of U.S. healthcare providers projected to integrate AI into their revenue cycle processes by 2028. These technologies will help reduce administrative burdens, improve claim accuracy, and optimize revenue management, driving market growth.
- Integration of Blockchain Technology: Blockchain technology is expected to play a larger role in the RCM market by 2028. Healthcare organizations will increasingly adopt blockchain to secure patient data, streamline claim submissions, and reduce fraud. Blockchains ability to provide a transparent and immutable ledger of healthcare transactions will help improve trust between providers and payers, fostering market growth.
Scope of the Report
|
By Product |
Integrated Solutions Standalone Solutions |
|
By End-User |
Hospitals Ambulatory Care Centers Physician Practices |
|
By Region |
North East West South |
Products
Key Target Audience Organizations and Entities Who Can Benefit by Subscribing This Report:
- Medical Billing Companies
- Insurance Companies
- Healthcare Investors
- Financial Institutions
- Government Regulatory Bodies (e.g., Centers for Medicare & Medicaid Services)
- Banks and Financial Institutions
- Private Equity Firms
- Venture Capitalist
Companies
Players Mentioned in the Report:
- Cerner Corporation
- McKesson Corporation
- Optum360
- Allscripts Healthcare Solutions
- GE Healthcare
- Athenahealth
- Conifer Health Solutions
- eClinicalWorks
- Experian Health
- Change Healthcare
- R1 RCM
- SSI Group
- NextGen Healthcare
- Kareo
- Greenway Health
Table of Contents
1. USA Revenue Cycle Management Market Overview
1.1. Definition and Scope
1.2. Market Taxonomy
1.3. Market Growth Rate
1.4. Market Segmentation Overview
2. USA Revenue Cycle Management Market Size (in USD Bn), 2018-2023
2.1. Historical Market Size
2.2. Year-on-Year Growth Analysis
2.3. Key Market Developments and Milestones
3. USA Revenue Cycle Management Market Analysis
3.1. Growth Drivers
3.1.1. Complexity of Healthcare Billing
3.1.2. Transition to Value-Based Care
3.1.3. Rising Healthcare Expenditure
3.1.4. AI and Automation Adoption
3.2. Restraints
3.2.1. High Implementation Costs
3.2.2. Regulatory Compliance
3.2.3. Data Security Concerns
3.2.4. IT Workforce Shortage
3.3. Opportunities
3.3.1. Outsourcing of RCM Services
3.3.2. Integration of Blockchain Technology
3.3.3. Cloud-Based RCM Solutions
3.4. Trends
3.4.1. AI-Driven Automation
3.4.2. Value-Based Care Adoption
3.4.3. Cloud-Based Platforms
3.5. Government Regulations
3.5.1. Medicare and Medicaid Reforms
3.5.2. Healthcare Transparency Initiative
3.6. SWOT Analysis
3.7. Stakeholder Ecosystem
3.8. Competition Ecosystem
4. USA Revenue Cycle Management Market Segmentation, 2023
4.1. By Product Type (in Value%)
4.1.1. Integrated Solutions
4.1.2. Standalone Solutions
4.2. By End-User (in Value%)
4.2.1. Hospitals
4.2.2. Ambulatory Care Centers
4.2.3. Physician Practices
4.3. By Region (in Value%)
4.3.1. North
4.3.2. South
4.3.3. East
4.3.4. West
5. USA Revenue Cycle Management Market Cross Comparison
5.1. Detailed Profiles of Major Companies
5.1.1. Cerner Corporation
5.1.2. McKesson Corporation
5.1.3. Optum360
5.1.4. GE Healthcare
5.1.5. Allscripts Healthcare Solutions
5.2. Cross Comparison Parameters (No. of Employees, Headquarters, Inception Year, Revenue)
6. USA Revenue Cycle Management Market Competitive Landscape
6.1. Market Share Analysis
6.2. Strategic Initiatives
6.3. Mergers and Acquisitions
6.4. Investment Analysis
6.4.1. Venture Capital Funding
6.4.2. Government Grants
6.4.3. Private Equity Investments
7. USA Revenue Cycle Management Market Regulatory Framework
7.1. Compliance Requirements
7.2. Certification Processes
8. USA Revenue Cycle Management Future Market Size (in USD Bn), 2023-2028
8.1. Future Market Size Projections
8.2. Key Factors Driving Future Market Growth
9. USA Revenue Cycle Management Future Market Segmentation, 2028
9.1. By Product Type (in Value%)
9.2. By End-User (in Value%)
9.3. By Region (in Value%)
10. USA Revenue Cycle Management Market Analysts Recommendations
10.1. TAM/SAM/SOM Analysis
10.2. Customer Cohort Analysis
10.3. Marketing Initiatives
10.4. White Space Opportunity Analysis
Disclaimer
Contact Us
Research Methodology
Step:1 Identifying Key Variables:
Ecosystem creation for all the major entities and referring to multiple secondary and proprietary databases to perform desk research around market to collate industry level information.
Step:2 Market Building:
Collating statistics on USA Revenue Cycle Management Market over the years, penetration of marketplaces and service providers ratio to compute revenue generated for USA Revenue Cycle Management Industry. We will also review service quality statistics to understand revenue generated which can ensure accuracy behind the data points shared.
Step:3 Validating and Finalizing:
Building market hypothesis and conducting CATIs with industry experts belonging to different companies to validate statistics and seek operational and financial information from company representatives.
Step:4 Research output:
Our team will approach multiple RCM software companies and understand nature of product segments and sales, consumer preference and other parameters, which will support us validate statistics derived through bottom to top approach from such RCM Software companies.
Frequently Asked Questions
01 How big is the USA Revenue Cycle Management market?
The USA Revenue Cycle Management (RCM) Market was valued at USD 155.78 billion. The market growth is driven by the increasing complexity of healthcare reimbursements, government regulations, and the rising need for effective financial management in healthcare institutions.
02 What are the challenges in USA Revenue Cycle Management market?
The major challenges faced by the USA Revenue Cycle Management Market are high implementation costs for smaller healthcare providers, complex regulatory requirements, data security concerns, and a shortage of skilled IT professionals. These challenges affect the adoption of advanced RCM systems, particularly for smaller institutions.
03 Who are the major players in the USA Revenue Cycle Management market?
The major players in the USA Revenue Cycle Management Market are Cerner Corporation, McKesson Corporation, Optum360, Allscripts Healthcare Solutions, and GE Healthcare.
04 What are the main growth drivers of the USA Revenue Cycle Management market?
The key drivers of growth in the USA Revenue Cycle Management Market include increasing complexity of healthcare reimbursements and the pressure on healthcare providers to streamline operations.
Why Buy From Us?

What makes us stand out is that our consultants follows Robust, Refine and Result (RRR) methodology. i.e. Robust for clear definitions, approaches and sanity checking, Refine for differentiating respondents facts and opinions and Result for presenting data with story

We have set a benchmark in the industry by offering our clients with syndicated and customized market research reports featuring coverage of entire market as well as meticulous research and analyst insights.

While we don't replace traditional research, we flip the method upside down. Our dual approach of Top Bottom & Bottom Top ensures quality deliverable by not just verifying company fundamentals but also looking at the sector and macroeconomic factors.

With one step in the future, our research team constantly tries to show you the bigger picture. We help with some of the tough questions you may encounter along the way: How is the industry positioned? Best marketing channel? KPI's of competitors? By aligning every element, we help maximize success.

Our report gives you instant access to the answers and sources that other companies might choose to hide. We elaborate each steps of research methodology we have used and showcase you the sample size to earn your trust.

If you need any support, we are here! We pride ourselves on universe strength, data quality, and quick, friendly, and professional service.